Smart Bandage Uses Electricity to Accelerate Wound Healing
A new smart bandage has been developed to speed up the wound healing process by actively monitoring and responding to the wound’s condition. This innovative device, called a-Heal, fits inside a commercial colostomy bandage and includes a camera that captures images of the wound every two hours. These images are sent wirelessly to a machine learning system that analyzes the wound and provides updated recommendations on how to stimulate healing effectively.
The a-Heal bandage was created by a multidisciplinary research team led by Marco Rolandi, a professor of electrical engineering and computer science at the University of California Santa Cruz. The initial goal was to reduce healing time for battlefield injuries by 50 percent, as part of a Defense Advanced Research Projects Agency (DARPA) initiative. Although the device was tested on a pig wound that heals quickly, Rolandi explains that a-Heal could also be used for wounds that are difficult to heal, such as chronic wounds or infected wounds.
How the Smart Bandage Uses Electricity and Machine Learning to Heal Wounds
Traditional wound dressings follow a one-size-fits-all approach and cannot adapt to the unique healing process of each wound. In contrast, a-Heal monitors wounds continuously, diagnoses the current healing stage, suggests appropriate treatments, and delivers those treatments directly to the wound. This creates a feedback loop that actively supports and accelerates healing.
The key to this process is a machine learning algorithm called ML Physician. It analyzes each wound image by comparing it to training data and determines the wound’s healing stage. The algorithm then decides if the wound is healing properly or if it requires intervention to speed up recovery. Based on these recommendations, the bandage activates bioelectronic actuators to deliver one of two treatments: electrical stimulation to reduce inflammation or infusion of fluoxetine, a drug that promotes tissue growth.
The device’s camera captures 11 images at different focal depths every two hours. Although it is unclear how well the camera performs on darker human skin tones, Rolandi notes that with appropriate training data, the system should work effectively. The machine learning algorithm uses a leader-follower strategy, where a component called Deep Mapper predicts what the wound should look like at the next imaging session. The system then adjusts treatment to follow this predicted healing path.
Initially, the bandage applies electrical stimulation. When the probability that the wound remains in the inflammatory stage drops to 40 percent, the treatment switches automatically to drug delivery. The wound healing process generally passes through four stages: blood clotting, inflammation, tissue growth, and maturation.
Smart Bandage Results and Future Developments
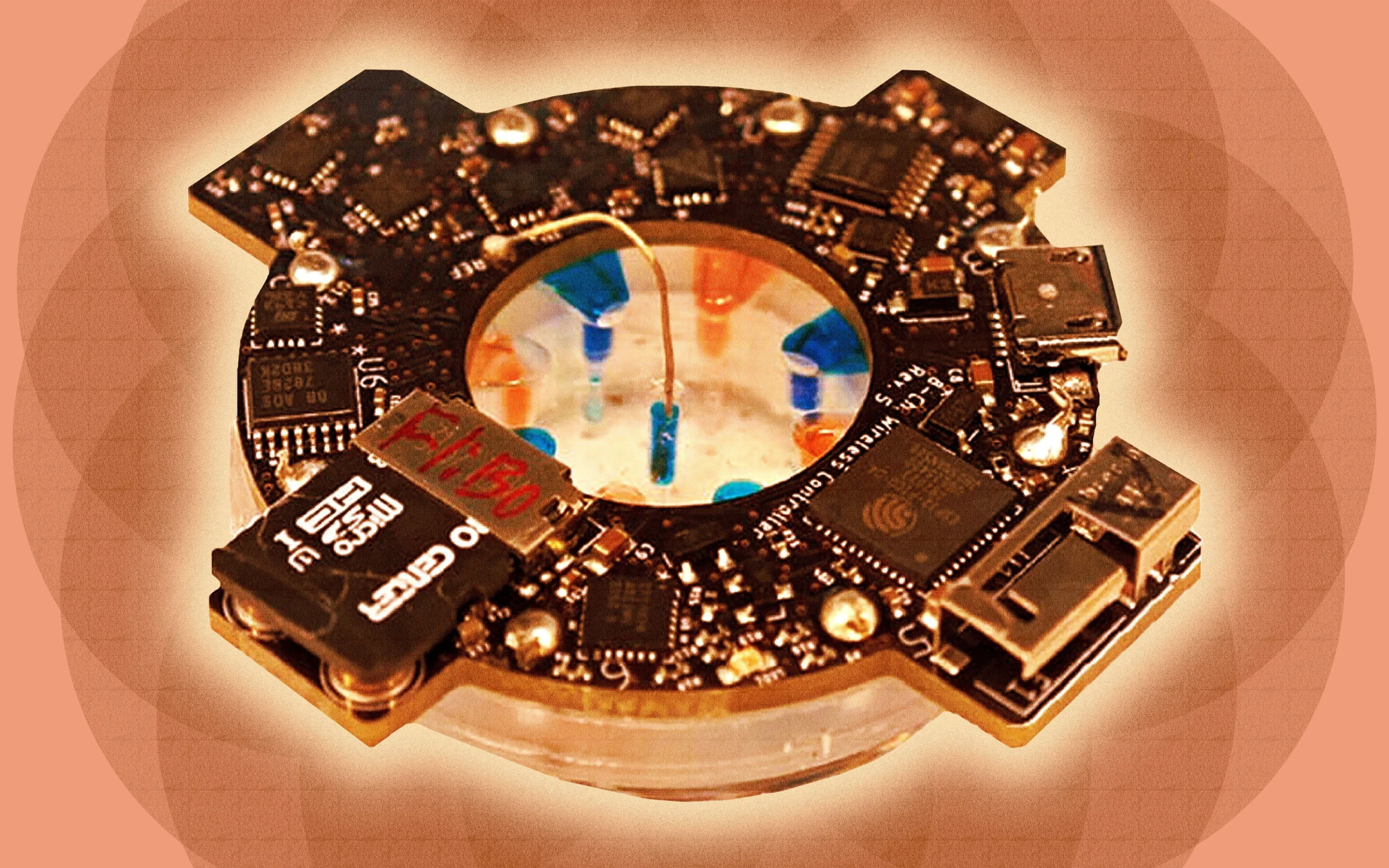
The bioelectronic actuator delivering treatments is a cylindrical silicone polymer with eight reservoirs arranged in a circle—four for electrical stimulation and four for drug delivery. Each reservoir contains an electrode, and a hydrogel connects the electrodes to the wound. Using iontophoresis, the device delivers either a saline solution for electrical stimulation or a fluoxetine drug solution. Rolandi explains that the device controls the dose precisely by measuring the electrical current, which corresponds to the number of therapy molecules entering the wound.
In tests on a pig, the smart bandage showed promising results. After seven days of treatment, 50 percent of the wound treated with the device was covered by new skin cells, compared to only 20 percent in the control wound. Additionally, the gene interleukin 1 beta, associated with inflammation, was reduced by 61 percent in treated wounds. Other genes related to inflammation and healing also showed positive trends, although the sample size was small and results were not yet statistically significant.
Experts not involved in the study, such as Geoffrey Gurtner, a physician and professor at the University of Arizona and Stanford University, noted that the combination of photographic monitoring and closed-loop treatment is a novel approach. While he described the effect as modest, he found the increased re-epithelialization encouraging. Gurtner also expressed interest in seeing future studies with larger sample sizes and longer treatment durations that follow wounds through full closure.
Rolandi explained that the team chose to treat wounds for only seven days in this initial study because early intervention has the most significant impact on healing. He also noted the complexity of conducting large animal preclinical trials. The researchers published their findings in Biomedical Innovations on September 23.
Looking ahead, the team plans to simplify the device, which currently takes about a month to build. They are developing a flexible version of the smart bandage, which they recognize as a necessary improvement for future clinical use.
Overall, the smart bandage uses electricity combined with machine learning to monitor and treat wounds in a personalized way, offering a promising new approach to accelerate healing.
For more stories on this topic, visit our category page.
Source: original article.